Digestive symptoms can derail daily life, limit meals, and sap energy. People often look for trustworthy information before discussing medications with a clinician. Domperidone sometimes comes up in those conversations, and it helps to understand what it is and what it is not.
If you are exploring background context, you can Learn About Domperidone through a product page while keeping the focus on education and safety. Use that information as a starting point, then bring your questions to a qualified healthcare professional who knows your history.
What it is and where it fits
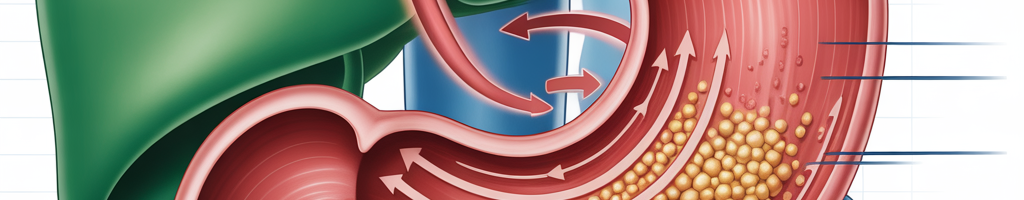
Domperidone is a prescription medicine that affects gut motility, which means how quickly food moves through the stomach. It also blocks certain dopamine receptors outside the brain, which can reduce nausea in some people. Different countries regulate it differently; access varies, and practices can shift as evidence evolves.
Because digestive conditions are complex, no single option suits everyone. A clinician weighs potential benefits against risks, other health issues, and your goals. The goal is relief without compromising long‑term safety or quality of life.
Symptoms and conditions that bring people to care
Slow stomach emptying and meal‑related distress
Some people experience early fullness, upper abdominal bloating, or uncomfortable fullness hours after eating. Others report nausea or vomiting after small meals. These symptoms can occur in gastroparesis, a condition marked by delayed stomach emptying, or in functional dyspepsia, which involves upper‑gut discomfort without obvious structural disease.
Tracking when symptoms occur matters. Do they intensify after high‑fat meals? Do liquids sit better than solids? A simple diary, including meals, portion sizes, timing, and symptoms, can give your clinician a clearer picture.
Cycles of nausea and vomiting
Nausea can be triggered by many issues, from migraines to medication effects. Some people notice patterns, like morning flares or flares during stress. Understanding triggers, hydration status, and recent medication changes can guide safer choices and set realistic expectations.
Every day has impacts that deserve attention
Digestive symptoms can affect sleep, social activities, and work. Anxiety around eating can lead to skipped meals, which may worsen fatigue and nutritional gaps. Name these impacts early; improving quality of life is a valid clinical goal.
Safety notes, side effects, and precautions
Common experiences and what to watch for
Some people taking a pro‑motility agent report dry mouth, headache, mild abdominal cramps, or dizziness. These are non‑specific and can overlap with the underlying condition. Keep a symptom log and note any sudden changes, especially during the first weeks of therapy or dose adjustments.
Heart rhythm considerations
A key safety point is the potential for effects on cardiac conduction, notably QT prolongation, which can raise the risk of arrhythmias. The personal baseline risk varies based on age, electrolyte levels, and coexisting heart conditions. Discuss any history of fainting, palpitations, or known arrhythmias and ask whether ECG monitoring makes sense for you.
Medication interactions
Some antibiotics, antifungals, and other drugs can increase blood levels of certain pro‑motility agents and raise rhythm risk. Other medicines also lengthen the QT interval, compounding the effect. Always share a complete list of prescriptions, over‑the‑counter products, and supplements, including grapefruit products, with your clinician and pharmacist.
Lactation and off‑label contexts
Domperidone has been discussed for lactation in some regions, but the practice remains controversial and regulated differently worldwide. The potential benefits must be weighed against maternal cardiac risk and other factors. People considering this path should work closely with clinicians who understand both lactation support and medication safety.
How clinicians often approach evaluation
History, exam, and targeted tests
A careful history often comes first: timing of symptoms, weight changes, hydration, and medication review. Depending on the situation, clinicians may order lab tests, check thyroid and blood sugar, or consider a gastric emptying study. The goal is to confirm patterns and rule out conditions that call for different strategies.
Layered care plans
Treatment plans are usually layered and tailored. They may combine meal strategy, symptom‑targeted therapies, and, in some cases, a pro‑motility medicine. Regular follow‑up allows fine‑tuning and helps catch side effects early.
Practical, evidence‑aware self‑care alongside medical guidance
Meal patterns and textures
Many people do better with smaller, more frequent meals spread throughout the day. Lower‑fat, lower‑fiber textures may be gentler when symptoms flare, since fat and roughage can slow stomach emptying. When symptoms settle, gradual re‑expansion of foods helps maintain variety and nutrition.
Hydration and nutrition basics
Steady hydration supports circulation and digestion. If solids are difficult, nutrient‑dense liquids or blended meals may bridge gaps. A dietitian familiar with upper‑GI conditions can suggest options that meet protein, vitamin, and mineral needs without worsening symptoms.
Trigger awareness and gentle activity
Noting individual triggers, such as spicy foods, carbonated drinks, or large late‑night meals, can cut down symptom spikes. Light movement after eating, like a short walk, may support digestion for some people. Leave 2–3 hours between the last meal and bedtime to reduce overnight discomfort.
When to pause and call a professional
Seek timely care for persistent vomiting, signs of dehydration, severe abdominal pain, blood in vomit, or unintended rapid weight loss. New chest pain, fainting, or palpitations warrant urgent evaluation. These symptoms can signal something different from everyday functional complaints.
Context, access, and equity
Access to gastroenterology care and specific medicines varies widely by location, insurance, and regulatory status. Some patients weigh travel, costs, and wait times when planning care. Discuss these realities openly; clinicians can often suggest interim strategies or monitoring plans that fit your situation.
People reading about pro‑motility options sometimes explore resources within the broader Gastrointestinal space to understand related conditions and non‑drug strategies. Keep the conversation grounded in your personal risks, your symptom pattern, and your values.
A brief, neutral note on cross‑border access: Some individuals explore Canadian pharmacies that ship to the US to navigate cost or availability concerns. Regulations and safety standards differ; independent verification and clinician involvement remain essential for any decision.
Questions to bring to your next appointment
- Given my symptoms and history, where does Domperidone fit among options?
- What baseline tests or monitoring do you recommend for cardiac safety?
- Which of my current medications or supplements could interact?
- If we try a pro‑motility medicine, what outcomes and timelines should I track?
- What non‑drug strategies can we prioritize alongside treatment?
Preparing these questions in writing can streamline the visit and build a shared plan. Clear goals, less nausea, better meal tolerance, or improved energy make it easier to measure progress and adjust care.
This content is provided for general education about digestive health and medication safety. For further reading about the company that hosts the resources, you can learn more at BorderFreeHealth , and then decide with your clinician how to interpret any information for your own care.
Medical disclaimer: This content is for informational purposes only and is not a substitute for professional medical advice.
In closing, digestive symptoms deserve attention and compassion, not dismissal. With careful assessment, pragmatic self‑care, and informed discussion, many people find steadier ground. If Domperidone enters the conversation, center safety, monitoring, and your goals are the guideposts.
Get 4 Free Sample Chapters of the Key To Study Book
Get access to advanced training, and a selection of free apps to train your reading speed and visual memory